This page was generated automatically. To view the article in its initial location, please navigate to the link below:
https://www.nature.com/articles/s41598-024-83607-w
Additionally, if you wish to have this article removed from our website, kindly reach out to us.
Fundamental characteristics of the participants
Table 1 illustrates the characteristics of the participants. Among 438,681 participants, 75,056 (17.11%) exhibited CMDs. Within this group, 15.12% had one CMD, 1.90% had two CMDs, and 0.09% had three CMDs. Those with one, two, or three CMDs were compared to individuals without any CMDs. The first group was older, had a higher proportion of males and retirees, lower educational levels, poorer economic conditions, reduced normal BMI rates, fewer carriers of the APOE ε4 gene, more instances of dyslipidemia and hypertriglyceridemia, as well as greater usage of lipid-lowering medications and aspirin. Moreover, this demographic exhibited a substantial prevalence of patients with moderate to severe serum 25(OH)D deficiency and hypertension, while presenting a relatively low prevalence of depression. Notable statistical discrepancies in exposure to ecological air contaminants and healthy lifestyle assessments were observed between individuals with and without CMDs, with a greater fraction of patients with CMDs exposed to moderate and high levels of ecological air pollutants in contrast to those without CMDs. Healthy lifestyle assessment scores of 0-1, 2-3, and 4 were elevated among individuals with CMDs compared to those without, while the proportion of scores ranging from 5-7 was diminished in patients with CMDs.
The likelihood of experiencing mild cognitive impairment, all-cause dementia, Alzheimer’s disease, and vascular dementia among patients with CMDs was 1.951, 1.554, 1.216, and 2.032 times greater, respectively, compared to those without CMDs [mild cognitive impairment: HR = 1.951, 95% CI: 1.404, 2.710; all-cause dementia: HR = 1.554, 95% CI: 1.473, 1.640; Alzheimer’s disease: HR = 1.216, 95% CI: 1.204, 1.228; vascular dementia: HR = 2.032, 95% CI: 1.799, 2.296]. The risk for developing mild cognitive impairment, all-cause dementia, Alzheimer’s disease, and vascular dementia appears to escalate with the increasing number of CMDs. Those with all three types of CMDs face the greatest risk of total dementia, Alzheimer’s disease, and vascular dementia (Table 2). Furthermore, the incidence rates of mild cognitive impairment, all-cause dementia, Alzheimer’s disease, and vascular dementia per 1,000 person-years were 0.038 (95% CI: 0.03, 0.04), 0.943 (95% CI: 0.92, 0.97), 0.455 (95% CI: 0.44, 0.47) and 0.155 (95% CI: 0.14, 0.17) for those without CMDs. In the CMDs population, the prevalence rates of mild cognitive impairment, all-cause dementia, Alzheimer’s disease, and vascular dementia per 1000 person-years were 0.064 (95% CI: 0.05, 0.08), 2.593 (95% CI: 2.50, 2.69) and 1.010 (95% CI: 0.95, 1.010), respectively (Table 3).
Impact of ecological air pollution on mild cognitive impairment and dementia risk in individuals with cardiometabolic diseases
When considering the combination of CMDs status and ecological air pollution factors, patients with non-CMDs as well as those with CMDs demonstrated consistent associations with a heightened risk of mild cognitive impairment, all-cause dementia, Alzheimer’s disease, and vascular dementia when maintaining high levels of exposure to ecological air pollution (Fig. 1). The risk for mild cognitive impairment, all-cause dementia, Alzheimer’s disease, and vascular dementia is 2.562 times, 1.686 times, 1.267 times, and 2.006 times higher, respectively, in patients with CMDs and significant exposure to ecological air pollution than in those without CMDs and minimal exposure (Table 4). Among these, elevated levels of exposure to PM2.5, PM2.5−10, PM10, NO2, and NOX may heighten the risk of various dementia subtypes among patients with CMDs (Tables S7). The rates of incidence for mild cognitive impairment, all-cause dementia, Alzheimer’s disease, and vascular dementia per 1000 person-years among individuals with CMDs who are exposed to high levels of ecological air pollution were 0.087 (95% CI: 0.06, 0.12), 2.699 (95% CI: 2.54, 2.86), 1.050 (95% CI: 0.95, 1.15), and 0.743 (95% CI: 0.66, 0.83), respectively (Tables S8).
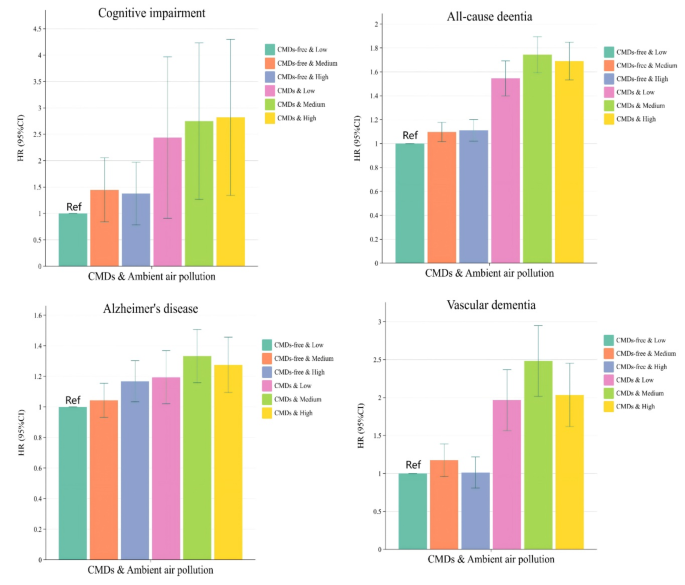
Correlation between ecological air pollution exposure and the likelihood of developing mild cognitive impairment and several dementia subtypes in patients with cardiometabolic disease. Abbreviations: CMDs, Cardiometabolic disease; HR, hazard ratios; CI, Confidence Intervals; In this model, we accounted for key sociodemographic factors [age, gender, ethnicity, educational attainment, occupational status, TDI, BMI] and health-related concerns [APOE genotype; history of hypertension; history of depression; dyslipidemia; hypertriglyceridemia; aspirin use; lipid-lowering medication use; serum 25(OH)D levels].
In the stratified analysis based on the presence of CMDs, elevated levels of ecological air pollution raised the likelihood of all-cause dementia and Alzheimer’s disease in the non-CMDs population by 12.0% and 25.3%, respectively [all-cause dementia: HR = 1.120, 95% CI:1.030,1.218; Alzheimer’s disease: HR = 1.253, 95% CI:1.123,1.398] (Table 5). In comparison with the lowest quartile of PM2.5 exposure, the likelihood of all-cause dementia and Alzheimer’s disease among individuals with non-CMDs exposed to the highest quartile of PM2.5 is 1.137 and 1.242 times greater, respectively (Tables S9). High ecological air pollution exposure augmented the risk of developing vascular dementia in patients with CMDs by 1.086 times compared to low exposure (Table 5). Additionally, ecological air pollution was…not identified to be correlated with the risk of acquiring mild cognitive impairment (P > 0.05) (Table 5 and Tables S9).
Impact of healthy lifestyle score on mild cognitive decline and dementia risk in people with cardiometabolic diseases
When evaluated together with CMDs status and healthy lifestyle score elements, if non-CMDs patients and those with CMDs upheld high healthy lifestyle scores, their likelihood of overall dementia, Alzheimer’s disease, and vascular dementia was reduced (Fig. 2). The likelihood of mild cognitive impairment and various dementia types diminished as healthy lifestyle scores rose in individuals both with and without CMDs. Those scoring between 5 to 7 and lacking CMDs exhibited the lowest risk for mild cognitive impairment, overall dementia, and vascular dementia. The likelihood of developing mild cognitive impairment, overall dementia, Alzheimer’s disease, and vascular dementia was 2.973-fold, 1.516-fold, 1.169-fold, and 1.940-fold greater, respectively, among individuals with CMDs and a healthy lifestyle score of 0 to 1 compared to those without CMDs and a healthy lifestyle score of 5 to 7 (Table 6). The rate of occurrences per 1000 person-years for mild cognitive impairment, overall dementia, Alzheimer’s disease, and vascular dementia among CMDs patients in the Healthy Lifestyle Score 0–1 category were 0.095 (95% CI: 0.02, 0.39), 2.951 (95% CI: 2.28, 3.82), 0.912 (95% CI: 0.57, 1.45), and 0.814 (95% CI: 0.49, 1.33), respectively (Table S10).
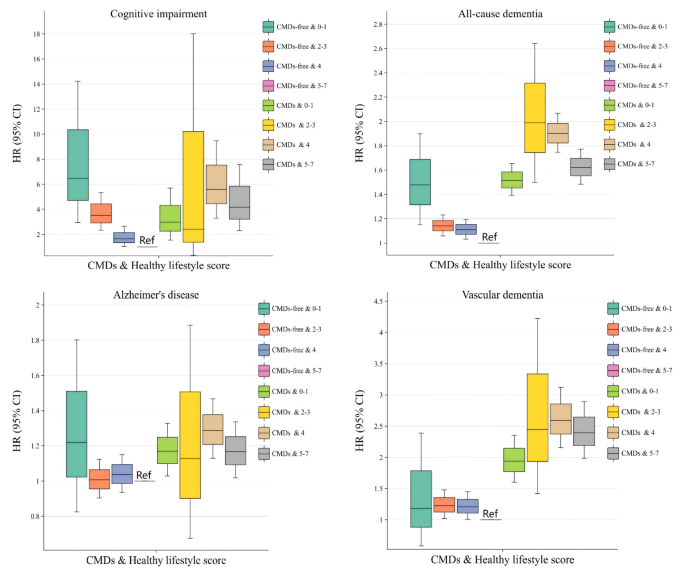
Relationship between healthy lifestyle score and the risk of developing cognitive impairment and various dementia subtypes in individuals with cardiometabolic disease. Abbreviations: CMDs, Cardiometabolic disease; HR, hazard ratios; CI, Confidence Intervals; In the model, we adjusted for fundamental sociodemographic variables [age, sex, race, education level, occupational status, TDI, BMI] and health-related factors [APOE genotype; history of hypertension; history of depression; dyslipidemia; hypertriglyceridemia; aspirin usage; lipid-lowering medication usage; serum 25(OH)D levels].
In research using the presence or absence of CMDs as a differentiating factor, a noteworthy statistical correlation was observed between a healthy lifestyle and the risk of incident overall dementia and vascular dementia in individuals with CMDs. The risk of developing overall dementia and vascular dementia was 1.314 and 1.354 times greater, respectively, in individuals with CMDs who scored 0 to 1 on the Healthy Lifestyle Score than those with CMDs scoring 5 to 7 (Table 7). Furthermore, barring the healthy diet model, significant statistical correlations were identified between the other six healthy lifestyle elements and the risk of developing mild cognitive impairment or various dementia subtypes. Regarding the magnitude of impact a healthy lifestyle has on the risk of developing mild cognitive impairment and dementia, adopting a healthy lifestyle might hold the greatest potential in decreasing the risk of mild cognitive impairment (Table S11).
Modification effect of ambient air pollution on mild cognitive impairment and dementia risk by lifestyle score in individuals with cardiometabolic diseases
In CMDs patients experiencing high levels of ambient air pollution, the likelihood of overall dementia may also lessen as the healthy lifestyle subgroup score ascends [0 to 1 score subgroup: HR = 3.049, 95% CI: 1.559, 5.965; 2 to 3 score subgroup: HR = 1.805, 95% CI: 1.534, 2.124; 4 score subgroup: HR = 1.525, 95% CI: 1.286, 1.808; 5 to 7 score subgroup: HR = 1.623, 95% CI: 1.383, 1.906] (Table 8). Corresponding findings were observed for the ecological pollutants PM2.5 and NOX (Table S12). CMDs individuals subjected to moderate air pollution exhibit the highest risk of vascular dementia within the categories of healthy lifestyle scores of 2–3, 4, and 5–7. Ambient air pollutants displayed a significantly detrimental effect on the risk of vascular dementia in individuals with CMDs compared to the non-CMDs population. Additionally, within the healthy lifestyle score 0 to 1 subgroup, no connections were discovered between CMDs patients exposed to high levels of ambient air pollution and the risk of developing mild cognitive impairment, Alzheimer’s disease, and vascular dementia (Table 8).
When examining the moderating influence of a healthy lifestyle on the effects of ambient air pollution on mild cognitive impairment and various dementia subtypes in populations with and without CMDs, it was observed that exposure to ambient air pollution might have a more pronounced effect on the risk of Alzheimer’s disease in non-CMDs patients within the 5 to 7 point category compared to the 2 to 3 point category of healthy lifestyle scores [2 to 3 score subgroup: HR = 1.267, 95% CI: 1.025, 1.566; 5 to 7 score subgroup: HR = 1.328, 95% CI: 1.123, 1.572] (Table 9). Moreover, in the healthy lifestyle score 0 to 1 subgroup, substantial statistical association was noted between PM2.5 and NOX exposure and the risk of overall dementia in CMDs patients. In the healthy lifestyle score 2 to 3 subgroup, a major statistical association was found between PM10 exposure and the risk of all-cause dementia and Alzheimer’s disease in CMDs patients (Table S13).
Concurrently, an interaction was discovered in this research between healthy lifestyle scores and exposure to ambient air pollution. Employing low-level exposure to ambient air pollution and a healthy lifestyle score of 5 to 7 as the reference group, it was concluded that exposure to medium-level ambient air pollution and a healthy lifestyle score of 0 to 1 among the non-CMDs population might present the highest risk for mild cognitive impairment and overall dementia. Conversely, exposure to elevated levels of ambient air pollution and a healthy lifestyle score of 0 to 1 in the CMDs population might yield the greatest risk of overall dementia and vascular dementia. This included a potential decrease in the risk for overall dementia and vascular dementia among patients with CMDs as healthy lifestyle scores improved at consistent levels of exposure to ambient air pollution (Table 10). Sensitivity analyses produced similar findings, reinforcing the study’s credibility (Table S14 to S25).
This page was generated automatically. To read the article in its original context, you can visit the link below:
https://www.nature.com/articles/s41598-024-83607-w
And if you wish to remove this article from our site, please contact us



