This web page was created programmatically, to learn the article in its unique location you may go to the hyperlink bellow:
https://www.kff.org/medicaid/challenges-with-implementing-work-requirements-findings-from-a-survey-of-state-medicaid-programs/
and if you wish to take away this text from our website please contact us
On July 4, President Trump signed into law a finances and tax invoice that features vital adjustments to the Medicaid program together with new necessities for states to implement work necessities for people enrolled by the Affordable Care Act (ACA) Medicaid growth pathway or sure state waivers. The Congressional Budget Office (CBO) estimates that this requirement could have the biggest impact on spending and protection in comparison with different provisions, lowering federal Medicaid spending by $326 billion over ten years and leading to 5.3 million extra people who find themselves uninsured.
In the summer season of 2025 whereas the brand new regulation was underneath debate in Congress and shortly after enactment, the 25th annual finances survey of Medicaid officers in all 50 states and the District of Columbia performed by KFF and Health Management Associates (HMA), in collaboration with the National Association of Medicaid Directors (NAMD) was within the area. To higher perceive how states are making ready for Medicaid work necessities, the survey requested states to debate anticipated challenges to implementing work necessities by the top of 2026, together with associated system adjustments and information matching. KFF anticipates that work necessities will apply to 43 states (41 growth states together with the District of Columbia plus Georgia and Wisconsin, which have expanded Medicaid by waivers). We acquired responses to this query from 42 of those states.
Because the survey query requested particularly about challenges pertaining to techniques, almost all states described system adjustments they anticipate to make; nonetheless, they recognized different challenges as properly. These challenges embody how rapidly the necessities have to be applied, workers capability considerations, value considerations, and points for candidates and enrollees (Figure 1). In many instances, states described a number of, interrelated challenges. For instance, the compressed implementation timeframe and want for federal steering usually factored into state responses detailing different challenges. Some states expressed extra challenges than others. Just a few states that had already been pursuing 1115 waivers to implement work necessities reported fewer anticipated implementation challenges. Understanding state challenges might help inform the content material and timing of forthcoming federal steering.
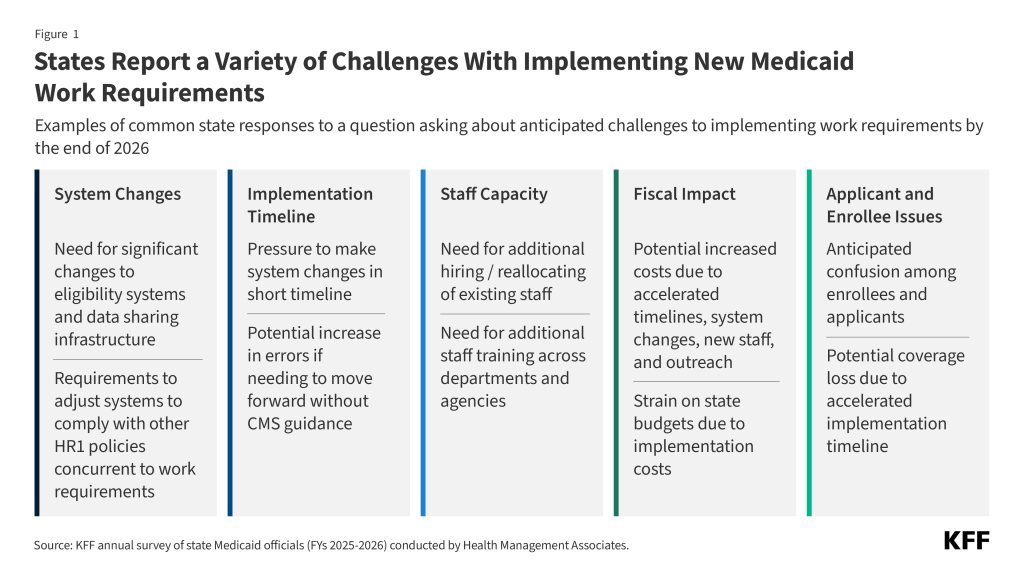
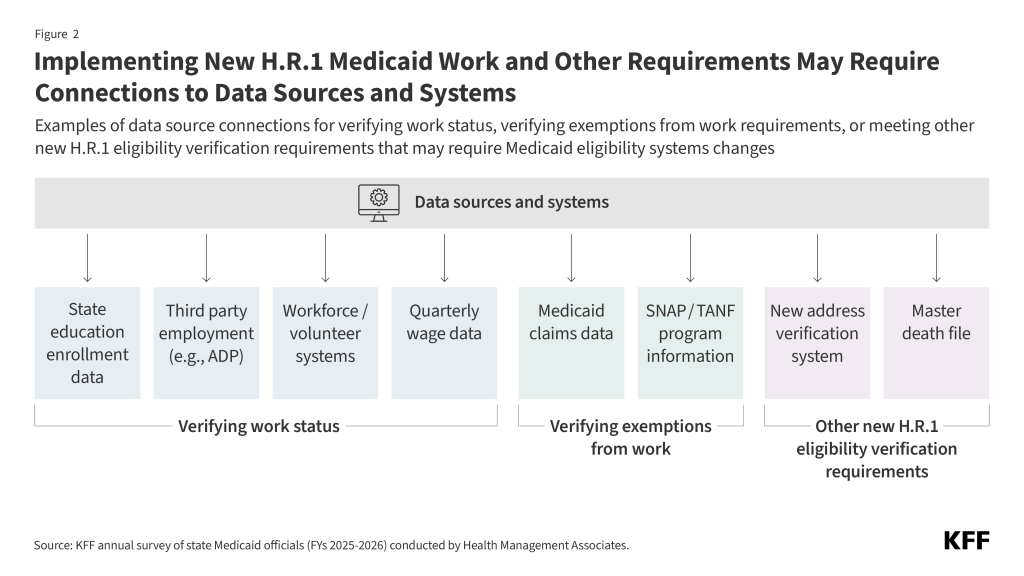
States cited the necessity to make main adjustments to eligibility techniques in a brief timeframe and the necessity for enhanced information sharing infrastructure as main challenges. States might want to make vital adjustments to eligibility techniques to have the ability to confirm compliance with work, college, and different qualifying actions in addition to to establish people who qualify for obligatory exemptions and elective exceptions. States expressed concern over having to make such main system adjustments in a really quick timeframe, noting the lengthy lead instances sometimes wanted to design, procure, and construct new techniques. Adding to the problem would be the have to make key system design and workflow choices earlier than CMS releases steering. Another precedence many states talked about is enhancing capabilities to gather and match information from a number of businesses and exterior sources (e.g., SNAP, Medicaid claims information, state training enrollment information) to cut back the burden on candidates and enrollees for documenting their work or exemption standing (Figure 2). However, some states acknowledged that information sharing infrastructure is restricted and establishing interfaces to precisely share information will take time to place in place.
According to a number of states, different coverage adjustments within the regulation, together with restrictions on eligibility for lawfully current immigrants, 6-month eligibility redeterminations for growth enrollees, and limits to retroactive Medicaid protection, additionally require vital techniques adjustments. Increasing this complexity, some states additionally talked about the problem of aligning totally different work necessities throughout Medicaid, SNAP, and TANF, in addition to having to make advanced techniques and eligibility coverage adjustments for SNAP as required by the brand new regulation. These adjustments could also be significantly sophisticated for states with built-in Medicaid and SNAP eligibility techniques. In addition, a number of states famous that they’re at the moment concerned in multiyear IT techniques tasks and that will probably be difficult to finish these tasks efficiently whereas additionally concurrently including new techniques redesigns. All of those techniques challenges are additional exacerbated by restricted state workers capability and monetary assets.
According to many states, the quick implementation timeline means they might want to transfer rapidly with key techniques adjustments and coverage choices earlier than clear federal steering is out there. States have simply over a yr to arrange to implement work necessities on January 1, 2027, and have lower than a yr earlier than they might want to start outreach to inform people of the brand new necessities in September 2026 (Figure 3). The regulation directs the Secretary of HHS to challenge an interim ultimate rule on implementing work necessities by June 1, 2026, leaving little time between when the steering is launched and when outreach begins. For many states, this quick timeline intensifies the strain to maneuver rapidly with system upgrades, significantly given the usually prolonged vendor procurement course of, and different key choices. However, a number of states emphasised the dangers of shifting ahead within the absence of clear steering, noting that if state choices are usually not aligned with the federal expectations, the ensuing rework would improve prices and probably delay assembly necessary deadlines. Some states described the implementation deadline as unrealistic, noting that it will increase the chance of errors that might result in pointless protection losses. In gentle of those dangers, some states mentioned early and clear steering from CMS can be useful, particularly on points such because the definition of medical frailty and different exemptions or the permissibility of self-attestation that might have an effect on techniques choices.
A small variety of states explicitly talked about curiosity within the possibility for states to pursue good religion waivers to delay implementation of labor necessities, noting that further steering can be wanted to know the standards to acquire a “good faith waiver” and the state software course of.
Figure 3
Several states reported workforce challenges, together with the necessity to rent or reallocate workers in anticipation of elevated workloads and the necessity for added workers coaching. Many states reported that they might want to rent further workers or reallocate present workers to deal with elevated workloads from verifications, appeals, and enrollee outreach. States additionally anticipate the necessity for added workers coaching, together with coaching workers throughout departments and businesses (e.g., SNAP), to make sure eligibility employees perceive the brand new guidelines and necessities, exemption standards, and documentation necessities. Just a few states known as out the extra workforce assets that will likely be essential to conduct complete and multi-modal outreach efforts and reply to the anticipated improve in enrollee inquiries.
Just a few states famous that workers are already managing main multiyear tasks which are underway, similar to eligibility system modernization tasks, forcing workers and management to juggle competing calls for. Similarly, restricted workers capability may trigger spillover results and lead to much less well timed eligibility determinations for enrollees not topic to work necessities.
Even with implementation funds and federal matching funds for administrative prices, some states cited the elevated prices of implementing work necessities as a priority. Numerous states explicitly talked about the fiscal implications tied to techniques adjustments, hiring further workers, and conducting outreach to enrollees. One state famous that, given the tight timeframe coupled with the enormity and complexity of the brand new necessities tied to system adjustments, interagency agreements, state rulemaking, and enrollee outreach, states may have to maneuver ahead on a number of parallel tracks, which may improve implementation prices and the chance for errors. Contracts for techniques adjustments or new elements are pricey, and states famous that accelerated timelines usually improve these prices. Some states additionally reported that the elevated prices will additional pressure already constrained state budgets. In addition, some states mentioned that new monetary penalties for error charges in SNAP and Medicaid could probably have an effect on how they transfer ahead with system adjustments. The new regulation supplies $200 million in funding to states for techniques growth, with states in a position to entry federal matching funds. The federal authorities generally provides 50 % of the funds for administrative actions however pays for as much as 90 % of sure administrative prices, together with for sure IT system adjustments.
While not requested straight about enrollee points, a number of states cited considerations for candidates and enrollees, together with anticipated confusion over the brand new necessities and attainable protection losses. States anticipate confusion amongst enrollees and candidates in regards to the new work necessities and listed educating people among the many challenges they are going to face. While states famous the significance of outreach to shoppers, a number of reported that efforts to maneuver ahead with communication and outreach with out federal steering may lead to extra enrollee confusion if CMS steering doesn’t align with state assumptions associated to documentation necessities, exemption definitions, or information matching. Some states additionally expressed concern over attainable protection loss stemming from the accelerated implementation timeline and indicated that they plan to research methods they will reduce any protection losses. One state famous explicit considerations for enrollees in rural areas with restricted web entry and people with jobs with fluctuating work hours.
This web page was created programmatically, to learn the article in its unique location you may go to the hyperlink bellow:
https://www.kff.org/medicaid/challenges-with-implementing-work-requirements-findings-from-a-survey-of-state-medicaid-programs/
and if you wish to take away this text from our website please contact us



