This page was generated programmatically; to access the article in its initial location, you can follow the link below:
https://pubmed.ncbi.nlm.nih.gov/39723991/
and if you wish to eliminate this article from our site, please reach out to us
Background:
Numerous childhood cancer survivors (CCS) experience treatment-associated late effects, which includes an elevated risk of obesity and metabolic syndrome. Maintaining a healthy way of life may mitigate the risk of related comorbidities. Consequently, CCS at risk could gain from lifestyle guidance during regular long-term follow-up (LTFU).
Objective:
We initiated a novel approach to diminish long-term morbidity among CCS and to acquire new perspectives on the lifestyles of these patients.
Methods:
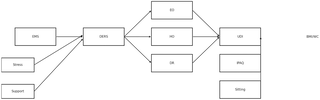
During a 1-year research period, lifestyle guidance was incorporated into LTFU management. Metabolic conditions, comprising hypercholesterolemia, diabetes mellitus, underweight or overweight, and low activity levels, were evaluated as criteria for screening various risk categories. The views of CCS, healthcare providers, and sports experts were contrasted to pinpoint those with the most significant needs. Every lifestyle consultation included general advice for physical activity, along with an evaluation of individual inclinations for and obstacles to adopting a healthier lifestyle. A follow-up session was conducted after 1 month.
Results:
Among the 155 CCS aged 18 to 63 years (n=100, 65% female and n=55, 35% male), 112 (72%) were identified as needing lifestyle counseling, as recognized by healthcare providers, sports experts, or the CCS themselves. Metabolic disorders impacted 45% (n=70) of these CCS, while 46% (n=72) did not achieve the suggested activity levels. In total, 120 (77%) CCS underwent lifestyle counseling, including 8 initially uninterested individuals who became receptive to suggestions. Those with a history of intensive cancer treatment exhibited the greatest necessity. A total of 65 (54%) CCS were recommended to alter their lifestyle in both domains (diet and physical activity), while 51 (43%) CCS received guidance solely for exercise (n=43 CCS, 36%) or diet (n=8 CCS, 7%). Four (3%) CCS, despite showing interest in counseling, did not receive any advice as they already adhered to the recommendations. Follow-up demonstrated high compliance with suggestions and successful incorporation into daily routines. In total, 97% (n=150) of survivors reported that the provision of lifestyle guidance during LTFU would be generally advantageous.
Conclusions:
Integrating specialized health care professionals, such as sports experts, into survivorship care enhances the multidisciplinary nature of LTFU management. Advocating for a healthy lifestyle through guideline-based lifestyle counseling is widely embraced among CCS and could reduce long-term morbidity.
Keywords:
cancer survivor; childhood cancer survivors; diabetes mellitus; health care professionals; healthy lifestyle; hypercholesterolemia; lifestyle counseling; long-term follow-up; metabolic disorders; metabolic syndrome; morbidity; patient; physical activity; risk of obesity; treatment-related.
This page was generated programmatically; to access the article in its initial location, you can follow the link below:
https://pubmed.ncbi.nlm.nih.gov/39723991/
and if you wish to eliminate this article from our site, please reach out to us